5 reasons why personal health budgets matter

5 Reasons PHBs Matter
The NHS Long Term Plan contains a commitment to deliver 200,000 Personal Health Budgets by 2023/24.
It was an ambitious target before Covid-19 struck and sounds even more challenging now.
With so many competing priorities, we ask could Personal Health Budgets be part of the solution rather than part of a problem?
#1> Balancing the Books - 10% Net Saving
According to the Office for National Statistics, the government will spend £280bn on measures to fight Covid-19 and its impact on the economy, in the current year alone. 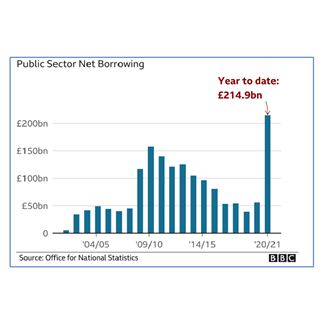
The public purse is stretched, and the conversations are starting about how we can all save money and attempt to balance the books. The evidence base on PHBs continues to evolve, and includes:
- NHS England analysis in 2019 of continuing healthcare PHBs across 11 CCGs which showed an aggregate net cost reduction in packages of care of 18% for cases where there was no change in assessed needs.
- NHS Midlands and Lancashire CSU analysis in 2017 of continuing healthcare PHBs across 17 CCGs which showed overall net savings of 17% between PHBs and conventional care package costs.
We have drawn on the above findings and our work with both local authorities and CCGs to develop a savings calculator for our Virtual Wallet PHB solution, which enables CCGs to identify and model their potential local savings. Saving estimates range from 5% to 25%, depending on the cohort and budget deployment model, but we would expect a CCG to be able to prudently forecast a net saving of at least 10% of the budget spend. In summary, PHBs are a proven way to make substantial cashable efficiencies, but it does take some time and effort and hence the need for CCGs to act now.
#2> The Aspiration Remains
Chapter one of the NHS Long Term Plan makes personalised care business-as-usual across the health and care system. Universal Personalised Care sets out how the NHS will systematically implement the Comprehensive Model for Personalised Care to reach 2.5 million people by 2023/24, of which a total of 200,000 people will be supported by PHBs by 2023/24.
At the end of 2019, some 80,000 PHBs were being reported (although many of them were personal wheelchair budgets).
One of the ways to achieve the 200,000 PHBs aspiration was making them the default position for Continuing Healthcare (CHC) packages, an expectation that was paused in March 2020 due to Covid-19.
The NHS has signalled that CCGs are expected to resume default position from September 2020, albeit subject to local capacity and readiness to support the delivery of PHBs.
The aspiration and the reinstatement of the default expectation are one perspective. Another way to approach this is from a demand viewpoint. It may not feel like it right now, but the focus on Covid-19 will pass and the public have become more attuned to - and interested in – personalised care than ever before, hence the need to get ahead of it, regardless of the targets themselves.
#3> Culture Shift - including Digital
 Chapter one of the NHS Long Term Plan identifies personalised care and digital as two of the five major, practical changes that will create the new NHS service model fit for the 21st century. Both of these represent seismic and challenging shifts in relation to people, processes and technology.
Chapter one of the NHS Long Term Plan identifies personalised care and digital as two of the five major, practical changes that will create the new NHS service model fit for the 21st century. Both of these represent seismic and challenging shifts in relation to people, processes and technology.
A publication by The Kings Fund entitled The road to renewal: five priorities for health and care identified ‘embedding and accelerating digital change in the wake of recent progress’ as one of the five priorities and stated: “Covid-19 … delivered an unprecedented shock to both demand for and supply of digital health services. The results have been substantial. In its recent history, the NHS has never seen such a rapid and widespread channel shift. The achievements of recent weeks stand in stark contrast to the relatively poor record the NHS has of adopting digital technologies at scale”.
One of the biggest challenges with an initiative like PHBs (and a concept like Virtual Wallet, our digital PHB solution) is that of culture change and transformation. Covid-19 has had horrific human costs, but is has acted as a catalyst for change in the NHS and in digital engagement. There is now an opportunity to embrace those changes for PHBs.
#4> Covid19 - Three opportunities for PHBs?
A publication by The Kings Fund entitled The road to renewal: five priorities for health and care identified ‘reshaping the relationship between communities and public services’ as one of the five priorities and stated: “The Covid-19 emergency has brought an upsurge in community solidarity and activism, underlining the vital role of local communities in supporting health and wellbeing”.
This is supported anecdotally by the 8pm clap, children leaving notes for elderly neighbours they barely know, people setting up social media groups to help with shopping for those shielding, the public signing up en masse for the NHS volunteering app and people generally helping their family, friends and neighbours more. Some of these movements have continued, some have waned.
One possibility for making some of them sustainable is to monetise them via PHBs – people could actually be paying their friends or neighbours to support them, if we open their eyes to it (promoting PHBs) and make it easy (like our Virtual Wallet PHB solution). It could solve some care and support needs whilst also addressing some of the unemployment issues affecting other sectors.
Secondly, we know that people are currently very wary of traditional care and support options (care homes and even domiciliary care) right now. The concept of employing a PA or finding non-traditional supports has never looked more enticing.
The Care Quality Commission found that admissions to care homes fell by more than a quarter among publicly funded clients and by two-thirds among self-funders, alongside a drop in the use of home care. People are voting with their feet, so there is a duty (opportunity?) to provide alternative options to people.
Thirdly, at a practical level, many places and services are closed right now, there are backlogs of referrals, labour shortages across the traditional health and social care sector and increased demand for services linked to mental health and long-covid. Some of the authorities we work with are responding to these challenges by offering fast-track personal budgets to people affected, and those people are embracing the chance to take control of what matters to them, and find more creative / rapid / effective ways of meeting their immediate care and support needs.
#5> PHBs work...and are the right thing to do!
 NHS England’s Universal Personal Care document states: “As well as being morally the right thing to do, a growing body of evidence shows that better outcomes and experiences, as well as reduced health inequalities, are possible when people have the opportunity to actively shape their care and support”.
NHS England’s Universal Personal Care document states: “As well as being morally the right thing to do, a growing body of evidence shows that better outcomes and experiences, as well as reduced health inequalities, are possible when people have the opportunity to actively shape their care and support”.
From tracking over 9,000 people with long-term conditions across a health and care system, evidence has shown that people who are more confident and able to manage their health conditions (i.e. have higher levels of activation) have 18% fewer GP contacts and 38% fewer emergency admissions than people with the least confidence.
An independent survey of 500 PHB holders in 2019 found that 78% of people would recommend a PHB to someone else.
NHS England’s Universal Personal Care document states: “This shift represents a new relationship between people, professionals and the health and care system. It provides a positive change in power and decision making that enables people to feel informed, have a voice, be heard and be connected to each other and their communities”.
This concept of empowerment sits at the heart of an emerging fundamental shift in the relationship between the citizen and the state. It is a global phenomenon, with personalised care models (and the equivalent of PHBs) becoming the norm in Australia, Canada and the USA, where our sister company is the market-leader in personalised care. Personalised care is the right thing to do, so we should do it now!
Agree?
We are passionate about PHBs. If you are too, get in touch for an informal discussion. We are happy to share our insights.
